Expert Care by Dr. Ankit Daware
Understanding the Occipitocervical Region
To understand the surgery better, it helps to know the anatomy. The occipitocervical region includes:
1. The Occiput
The occipital bone sits at the base of the skull. It connects directly with the first cervical vertebra (C1).
2. The Cervical Vertebrae (C1 & C2)
C1 (Atlas) allows the head to nod up and down.
C2 (Axis) enables the head to rotate side to side.
These two vertebrae work together to provide a combination of mobility and stability. They also protect the upper part of the spinal cord and brainstem.
3. Ligaments and Muscles
Strong ligaments hold the head and neck in proper alignment. Any disruption—through injury or disease—can lead to instability.
Because this region supports both movement and neurological function, conditions affecting it can quickly become serious.
What Is Occipitocervical Instability?
Occipitocervical instability occurs when the connection between the skull and upper cervical vertebrae becomes weak, loose, or damaged. As a result, the spinal cord or brainstem may become compressed, leading to neurological symptoms.
Patients may face:
Severe pain
Loss of balance
Difficulty supporting the head
Numbness or weakness
Breathing or swallowing difficulties (in advanced cases)
To prevent progressive neurological damage, stabilization through Occipitocervical Fusion Surgery is often recommended.
Conditions That Require Occipitocervical Fusion
Several medical conditions can cause instability at the occipitocervical junction. Dr. Ankit Daware treats all major causes with high precision.
1. Traumatic Injuries
High-impact accidents, falls, or sports injuries may fracture the occiput or upper cervical vertebrae.
2. Rheumatoid Arthritis
Severe arthritis can weaken ligaments, causing instability and spinal cord compression.
3. Congenital Anomalies
Some individuals are born with abnormalities like:
Atlantoaxial instability
Basilar invagination
Chiari malformation
These may require fusion to correct alignment.
4. Tumors
Tumors in the skull or cervical spine may weaken bone structures, requiring stabilization after removal.
5. Infections
Spinal infections like tuberculosis, osteomyelitis, or meningitis can damage bone and ligaments.
6. Degenerative Conditions
Age-related changes may cause instability when the structures lose strength.
Common Symptoms of Occipitocervical Problems
Patients usually experience symptoms such as:
Persistent neck pain
Severe headache at the back of the head
Difficulty rotating or supporting the head
Numbness, tingling, or weakness in arms
Balance problems
Swallowing difficulty
Visual disturbances
Gait instability
Reduced fine motor skills
If the spinal cord is severely compressed, symptoms may progress to:
Breathing issues
Loss of bowel or bladder control
Paralysis
Early diagnosis and treatment can prevent worsening symptoms.
Diagnosis of Occipitocervical Instability
Dr. Ankit Daware follows a systematic diagnostic approach to identify the cause and severity of instability:
1. Clinical Examination
Evaluation of:
Neck mobility
Muscle strength
Reflexes
Sensation
Neurological deficits
2. Imaging Tests
To confirm the diagnosis, tests include:
X-rays (flexion and extension views)
CT scan for bone details
MRI for spinal cord and nerve assessment
Dynamic scanning to check for movement-related instability
Each test plays a key role in planning a safe and effective surgical treatment.
Non-Surgical Treatment Options
Before recommending surgery, Dr. Daware may suggest conservative methods if the condition is mild.
These may include:
Cervical collars or braces
Physiotherapy to strengthen muscles
Anti-inflammatory medications
Avoiding strenuous activities
However, if instability threatens the spinal cord or brainstem, surgery becomes essential to prevent long-term damage.
What Is Occipitocervical Fusion Surgery?
Occipitocervical Fusion is a surgical procedure that permanently stabilizes the junction between the skull and the cervical spine by connecting them with rods, screws, and bone grafts.
Purpose of the Surgery
To prevent spinal cord compression
To restore alignment
To stabilize fractures
To support the neck and head
To relieve pain and neurological symptoms
While it reduces neck movement to a certain degree, it significantly improves safety and quality of life.
How the Surgery Is Performed – Step-by-Step
Dr. Ankit Daware uses advanced surgical techniques, ensuring maximum precision and safety. The procedure typically involves the following steps:
1. Anesthesia & Positioning
Patients are given general anesthesia. They are positioned face-down to allow access to the upper cervical spine.
2. Surgical Incision
A small incision is made at the back of the head and upper neck.
3. Exposure of Bone Structures
Muscles are gently moved aside to reveal the occiput, atlas, and axis.
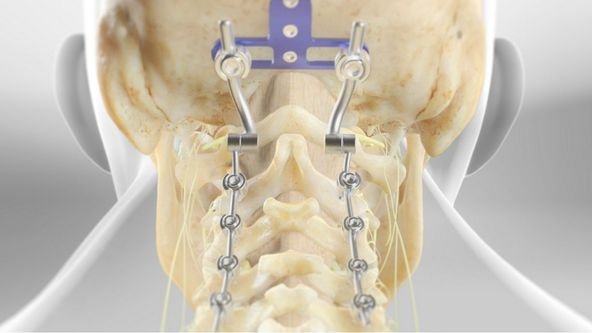
4. Screw Placement
Specially designed screws are inserted into:
The occipital bone
C2 (and sometimes C3) vertebrae
These screws allow controlled stabilization.
5. Rod Fixation
Titanium rods connect the screws, creating a stable framework.
6. Bone Grafting
Bone graft (either from the patient or donor) is added to promote natural bone fusion over time.
7. Final Stabilization
The alignment is checked, rods are tightened, and muscles/skin are sutured back.
8. Recovery Monitoring
Patients are observed in a controlled environment until stable.
Benefits of Occipitocervical Fusion
Patients experience several advantages after undergoing the surgery:
Improved neck stability
Relief from severe pain
Protection of the spinal cord and brainstem
Prevention of progressive neurological decline
Correction of deformities
Improved mobility and balance
Long-lasting structural support
Although the surgery slightly reduces neck mobility, the benefits far outweigh the limitations.
Recovery After Occipitocervical Fusion
Recovery varies depending on age, condition, and overall health. Dr. Daware provides individualized post-operative care for optimal healing.
Typical Recovery Timeline
Hospital Stay
2–5 days after surgery.
First 2 Weeks
Pain gradually reduces
Incision heals
Light activities allowed
4–6 Weeks
Use of cervical collar if recommended
Gradual strengthening exercises begin
3 Months
Most patients return to routine activities
Bone fusion begins to solidify
6–12 Months
Complete fusion achieved
Permanent stability established
Post-Surgery Guidelines
Avoid heavy lifting
Avoid sudden neck movements
Attend physiotherapy
Maintain good posture
Follow up regularly
Proper care ensures smooth recovery and long-term success.
Frequently Asked Questions
1. Is Occipitocervical Fusion a safe surgery?
Yes. When performed by an expert spine surgeon, it has a high success rate and significantly reduces the risk of spinal cord injury.
2. Will neck movement be limited after the surgery?
Yes, some movements—especially nodding and rotation—may reduce, but patients adapt well over time.
3. How long does the surgery take?
Typically between 2–3 hours.
4. When can I return to work?
Most patients resume normal desk work in 4–6 weeks. Physically demanding jobs may require 3–4 months.
5. Will I need physiotherapy?
Yes. Physiotherapy is essential for strengthening muscles and improving posture.
6. Is the hardware permanent?
Yes, the rods and screws remain in place to ensure long-term stability.
7. When does the fusion become fully solid?
Between 6 to 12 months, depending on bone quality.
