What Is Lumbar Decompression Surgery?
Lumbar decompression is a surgical procedure designed to relieve pressure on the spinal cord or spinal nerves in the lower back (lumbar spine).
This pressure typically arises from:
Herniated discs
Spinal stenosis
Degenerative disc disease
Spondylolisthesis
Bone spurs
Thickened ligaments
When spinal nerves are compressed, patients experience symptoms such as persistent back pain, numbness, tingling, radiating pain to the legs, difficulty walking, or even loss of bladder/bowel control.
Lumbar decompression aims to remove or reduce the structures causing compression so that the nerves can function normally again.
Why Is Lumbar Decompression Needed?
The lumbar spine carries most of the body’s weight, making it prone to age-related wear and tear. As the discs and joints degenerate, the space meant for the nerves narrows.
You may need lumbar decompression if:
Pain persists for more than 3–6 months
You experience radiating leg pain (sciatica)
You have numbness or weakness in the legs
Walking becomes difficult
Physiotherapy, medication, and injections fail
You experience severe nerve compression signs
Delaying the surgery may worsen nerve damage, which sometimes becomes irreversible. Early intervention ensures better recovery.
Symptoms That Indicate Need for Surgery
Patients typically present with:
Chronic low back pain
Leg pain or shooting pain (sciatica)
Numbness or tingling in legs or feet
Difficulty standing or walking
Muscle weakness
Tightness in hamstrings or calves
Loss of balance
Severe nerve compression symptoms, such as inability to control bladder or bowel
If you experience these symptoms, consultation with Dr. Ankit Daware is highly recommended.
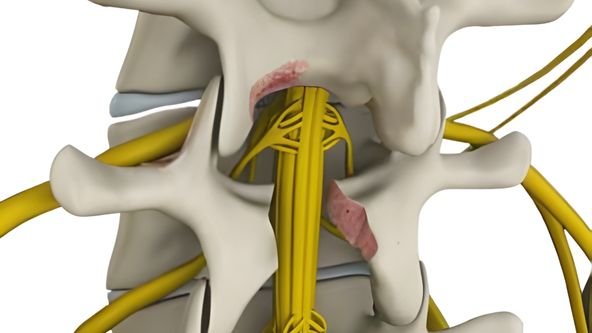
Causes of Lumbar Nerve Compression
1. Lumbar Spinal Stenosis
Narrowing of the spinal canal reduces space for nerves.
2. Herniated or Bulging Disc
The disc’s soft center protrudes and presses on the nerves.
3. Degenerative Disc Disease
Includes age-related changes causing back stiffness and nerve compression.
4. Spondylolisthesis
One vertebra slips over another, compressing nerves.
5. Bone Spurs (Osteophytes)
Bony overgrowth caused by arthritis.
6. Traumatic Injury
Accidents may damage spinal structures.
7. Thickened Ligaments
Ligamentum flavum thickens and reduces nerve space.
Types of Lumbar Decompression Surgery by Dr. Ankit Daware
Dr. Daware selects the surgical method based on MRI findings, severity of compression, and patient condition.
1. Laminectomy
A portion of the vertebral bone (lamina) is removed to free up the spinal canal.
2. Microdiscectomy
Removes the herniated portion of the disc pressing on the nerve.
Performed with microscopic precision and minimal incision.
3. Foraminotomy
Expands the foraminal canal, the doorway through which spinal nerves exit.
4. Laminotomy
Only a small portion of the lamina is removed, minimizing bone loss.
5. Minimally Invasive Lumbar Decompression (MIS-LD)
Uses advanced tools and keyhole incisions for faster recovery and less pain.
6. Spinal Fusion (if required)
Added in cases of instability like severe spondylolisthesis.
Dr. Ankit Daware emphasizes minimally invasive techniques whenever possible, ensuring quicker discharge, less bleeding, and early mobilization.
Pre-Surgery Evaluation
Before recommending surgery, Dr. Daware performs a comprehensive evaluation:
Detailed medical history
Neurological examination
MRI or CT scan
X-rays
Review of previous treatments
Discussion of lifestyle and occupational demands
This ensures that surgery is recommended only when truly necessary.
Procedure: How Lumbar Decompression Surgery Is Performed
1. Anesthesia
The procedure is usually performed under general anesthesia.
2. Positioning
Patient is positioned face-down for easy access to the spine.
3. Minimal Incision
In minimally invasive surgery, incisions are typically 1–2 cm.
4. Access to the Spine
Dilators or a tubular retractor create a path to the spine without damaging muscles.
5. Removal of Compressive Structures
Depending on the case:
Herniated disc piece is removed
Lamina portion is shaved
Ligament thickening is trimmed
Bone spurs are removed
6. Ensuring Nerve Freeing
Surgeon checks that nerves have adequate space.
7. Closure
Incisions are closed with minimal sutures.
8. Recovery Room
Patient awakens and recovery begins immediately.
Benefits of Lumbar Decompression Surgery
1. Relief from chronic back and leg pain
Most patients feel immediate relief from sciatica after the surgery.
2. Improved mobility
Walking, bending, and everyday activities become easier.
3. Better nerve function
Tingling, numbness, and weakness reduce significantly.
4. Return to normal life
Patients often resume work within days to weeks, especially with minimally invasive surgery.
5. Prevents permanent nerve damage
Timely surgery stops long-term complications.
Recovery After Lumbar Decompression
1. Hospital Stay
Most patients go home within 24–48 hours
(MIS patients may discharge the same day).
2. Pain Management
Medication is provided only as needed.
3. Physiotherapy
Begins immediately to strengthen the spine.
4. Activity Guidelines
Avoid lifting heavy weights for 6 weeks
Walk daily for faster healing
Avoid bending and twisting early on
5. Return to Work
Desk job: 1–2 weeks
Moderate work: 3–4 weeks
Hard physical work: 6–12 weeks
6. Long-Term Results
Most patients experience complete or near-complete recovery within 3 months.
