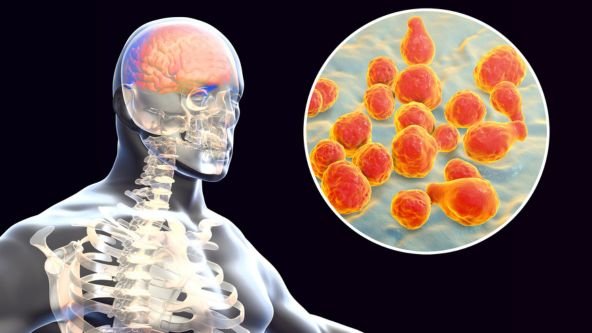
Meningitis is the inflammation of the meninges—the three layers of membranes (dura mater, arachnoid mater, and pia mater) that protect the brain and spinal cord. When these membranes become swollen or infected, it affects the functioning of the central nervous system, leading to potentially severe health issues.
Depending on the underlying cause, meningitis can be acute, subacute, or chronic.
Acute meningitis develops suddenly and progresses quickly.
Chronic meningitis develops gradually and may last for several weeks.
Early recognition and prompt medical treatment significantly reduce the risk of long-term complications.
Types of Meningitis
Meningitis can be classified into several categories based on the cause:
1. Bacterial Meningitis
This is the most severe form of meningitis. Bacterial meningitis requires urgent medical attention and hospitalization.
Common bacteria causing meningitis include:
Streptococcus pneumoniae
Neisseria meningitidis (Meningococcal meningitis)
Haemophilus influenzae type b (Hib)
Listeria monocytogenes
Group B Streptococcus (in newborns)
Without immediate treatment, bacterial meningitis can lead to brain damage, hearing loss, or death within hours.
2. Viral Meningitis
Viral meningitis is more common and usually less severe. Most people recover completely without lasting damage.
Viruses responsible include:
Enteroviruses
Herpes simplex virus
Varicella-zoster virus
Mumps virus
HIV
Although less dangerous than bacterial meningitis, viral meningitis still needs medical evaluation for proper care.
3. Fungal Meningitis
This type is rare but serious, usually affecting people with weakened immunity.
Common fungi causing meningitis:
Cryptococcus
Histoplasma
Coccidioides
Treatment involves long-term antifungal medications.
4. Parasitic Meningitis
Less common but can be life-threatening. One type, Naegleria fowleri, causes “brain-eating amoeba” meningitis, which is rare but often fatal.
5. Non-Infectious Meningitis
Caused by:
Certain medications
Autoimmune diseases
Cancer
Head injury
Brain surgery
Treatment focuses on the underlying cause.
Causes of Meningitis
The primary causes include:
Infections
Bacterial
Viral
Fungal
Parasitic
Non-infectious Causes
Autoimmune disorders like lupus
Cancer infiltrating the meninges
Reaction to medications (NSAIDs, antibiotics, chemotherapy drugs)
Post-surgical inflammation
Head trauma
Understanding the cause is essential for correct treatment.
Signs and Symptoms of Meningitis
Symptoms can vary depending on age and the type of meningitis.
Common Symptoms in Adults
High fever
Severe headache
Neck stiffness
Nausea and vomiting
Sensitivity to light (photophobia)
Confusion or altered consciousness
Seizures
Fatigue or difficulty waking up
Skin rashes (common in meningococcal meningitis)
If you or someone you know experiences these symptoms, immediate medical help is required.
Symptoms in Babies and Children
Infants may show different symptoms:
Constant crying
Poor feeding
Fever
Stiff neck or body
Bulging soft spot (fontanelle)
Irritability
Seizures
Difficulty waking up
Because symptoms can be subtle, medical evaluation is essential.
How Is Meningitis Diagnosed?
Accurate diagnosis is critical for effective treatment.
Dr. Ankit Daware uses advanced diagnostic tools to determine the type and cause of meningitis.
1. Physical Examination
Checking for:
Fever
Neck stiffness
Mental status changes
Rash
Neurological signs
2. Lumbar Puncture (Spinal Tap)
This is the most important test for meningitis. It analyzes cerebrospinal fluid (CSF) to detect:
Infection type
Inflammatory markers
Bacteria, viruses, fungi
3. Blood Tests
To identify infection in the bloodstream.
4. Imaging
CT scan
MRI
Used to detect swelling, abscesses, or complications.
5. PCR & Culture Tests
To identify specific organisms.
Timely and accurate diagnosis ensures proper treatment and reduces the risk of complications.
Treatment Options for Meningitis
Bacterial Meningitis Treatment
This form is a medical emergency.
Treatment includes:
Intravenous (IV) antibiotics
Corticosteroids to reduce brain inflammation
Fluids and electrolytes
Oxygen support if required
Medication for seizures
Monitoring in ICU (in severe cases)
Early treatment can be lifesaving.
Viral Meningitis Treatment
Most cases resolve on their own.
Treatment focuses on:
Bed rest
Hydration
Pain management
Antiviral medications (in specific viral infections)
Fungal Meningitis Treatment
Requires:
Long-term IV antifungal therapies
Monitoring of CSF and nervous system function
Possible Complications of Meningitis
If not treated promptly, meningitis can cause severe complications, such as:
Hearing loss
Brain damage
Memory difficulties
Seizures
Learning disabilities
Balance and coordination problems
Kidney failure
Shock
Loss of limbs (rare but seen in meningococcal meningitis)
Early diagnosis and treatment reduce these risks significantly.
Prevention of Meningitis
Several preventive steps can protect you and your family.
1. Vaccination
Vaccines available include:
Meningococcal vaccine
Pneumococcal vaccine
Hib vaccine
MMR (Measles, Mumps, Rubella) vaccine
Varicella (chickenpox) vaccine
Vaccination is the most effective preventive measure.
2. Good Hygiene Practices
Wash hands regularly
Avoid sharing drinks or utensils
Maintain clean surroundings
3. Strengthen Immunity
Healthy diet
Adequate sleep
Regular exercise
Stress management
4. Protect High-Risk Individuals
Infants, elderly people, and immune-compromised individuals require extra care.
